New NHS guidelines for HEPA-based air purification solutions

Summary
On the 9th of May 2023, National Health Service (NHS) England published new guidelines and standards for the application of HEPA filters for air cleaning in healthcare spaces, which is an addendum to the HTM-03-01 specialised ventilation advice and guidance for healthcare buildings. Considering recent ventilation challenges caused by COVID-19 and other infections, Healthcare trusts are under pressure to significantly improve ventilation, particularly in older hospitals and other healthcare settings such as primary care and dental suites, to protect patients, staff and visitors.
Local air cleaners utilising HEPA filtration were identified as an option to improve and supplement ventilation in NHS facilities that currently have non-existing or poorly performing and inadequate systems. This newly published interim guidance has been written to set basic standards regarding the effectiveness, performance validation, efficient airflow, maintenance, noise level and safety compliance required for portable (located at any suitable position in a room) and semi fixed (wall- or ceiling-mounted) HEPA filter devices to be utilised in healthcare and patient-related settings to reduce the risk of airborne transmission. This standard will assist trusts in selecting and implementing good quality, reliable equipment from trusted manufacturers.
Rensair welcomes this news as the updated guidelines set tighter standards for air purification in the healthcare sector, that it has already been adhering to for a very long time even before these recommendations were set out by the NHS. The Liverpool biovalidation protocol for air purifiers defined by the NHS Innovation Agency and the Office for Life Science and executed by Royal Liverpool University Hospital, showed that the efficiency of Rensair air purifiers far exceeded the NHS base standards. With the right technology and air purification and smart ventilation solutions public healthcare will be able to improve indoor air quality and infection prevention.
Effectiveness
Filter efficiency defines the fraction of particles removed and varies by size of particle with the most difficult size of particles of 0.3 μm, known as the most penetrating particle size (MPPS), as a leading indicator to declare a filter’s effectiveness. High Efficiency Particulate Air Filters (HEPA) with an efficiency of at least 99.95% (H13 filter) or 99.995% (H14 filter) for the MPPS under BS EN 1822-1 or ISO 29463-1 standards are recommended in the Healthcare sector. Nonetheless, performance in situ is sometimes lower depending on the filter and device design and the air flow rate why real-time tests provide a better understanding of a device’s ultimate performance. Emerging technologies such as ionisation, photocatalytic oxidation, electrostatic precipitation or others similar alongside filters, which are still lacking independent research, are not currently recommended for healthcare use unless there is clear evidence for both effectiveness and safety provided by manufacturers.
Filter-based air cleaning devices containing grades of filter lower than H13 or H14 may be appropriate for non-clinical areas and are not recommended for its use in settings with vulnerable patients. HEPA filter-based devices often also incorporate a coarse grade of filter to act as a dust filter or a carbon filter to manage odours and volatile organic compounds. Some devices may even contain several separate filters, while others incorporate the different stage filters into a single cartridge type unit. Complying with the safety requirements of the NHS, HEPA filter-based devices may also use germicidal ultraviolet (UVC) light alongside HEPA filters whose combination is likely to be effective. Such devices which incorporate other technologies should not produce ozone levels or other chemical pollutants in excess of the UK Workplace Exposure Limit (WEL) for ozone of 0.2 ppm after a 15 minute reference period.
Performance validation
Manufacturers should provide evidence that the HEPA filter used within the device meets BS EN 1822-1/ISO 29463-1 or equivalent standards and that the air cleaning device with filters in situ has been tested to an appropriate protocol that demonstrates how the device is likely to perform in a typical healthcare setting. As the performance of a HEPA filter is determined by the size of particles rather than the species of microorganism, it is not necessary for a manufacturer to conduct validation tests using microorganisms and can be carried out using inert particles of an appropriate size, usually in the 0.5–2 μm size range. Performance data including airflow rate through the device, filter pressure drop and measured impact of the device on particle concentration in a suitable test environment should be provided for each operational fan speed and for the MPPS achieving at least a 99% (2 log) reduction in a single pass through. To avoid potential leakage around the edge of the filter leading to underperformance of the device, a verification test has to be carried out by a qualified person or should be measured automatically within the device on first installation, after every filter change and when the device is being moved using the pressure drop method across the filter. Verification checks ensure that the performance of the device is maintained in between maintenance periods.
Efficient Airflow
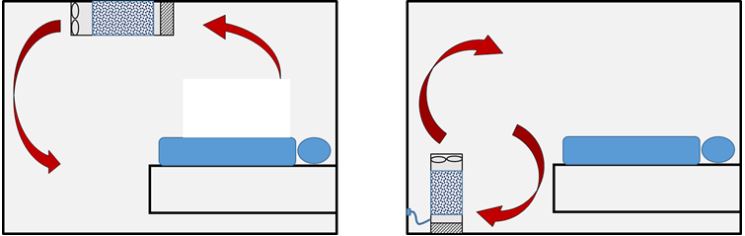
HEPA air cleaner devices’ performance depends on both the flow rate through the HEPA filter and the way the device distributes the air in a room. Both are important factors for ensuring devices are effective and properly positioned. HEPA filter-based air cleaners can be operated as a sole solution or in combination with an existing mechanical system or natural ventilation. Combinated solutions are recommended in healthcare settings to ensure sufficient outdoor air intake for the dilution of medical gases and noxious odours as well as to maintain appropriate levels of oxygen and carbon dioxide in accordance with the Building Regulations Part F. As an example, a treatment room with 6 ACH could achieve the equivalent of 10 ACH by installing a local filtration unit which recirculated and cleaned the equivalent of 4 eACH (equivalent Air Changes per Hour) to meet the requirements that comply with HTM-03-01. The number of devices required will be dictated by the existing background levels of ventilation.
The air processing capacity of filter-based devices is described by some manufacturers in terms of a Clean Air Delivery Rate (CADR) which is usually expressed in metres cubed per hour (m3h-1). Where a CADR is given it should be derived from measurements of how well the device removes a defined size of particles in a test room environment. CADR is a function of the airflow rate through the device, the quality of the filter and the way the device distributes air in a standardised test room. For that reason, it is important to understand that the actual performance in a real-world application will depend on the particular location and operation of the device, including the room size, layout, background ventilation, device design and maintenance. It is not recommended to use an air cleaning device with a lower grade of filter even if the quoted CADR is high, as the device may be less effective against the smallest pathogen carrying particles. Some manufacturers also adopt other metrics such as the time to reduce particle concentrations in a room by a specific percentage.
Going one step further in the future, the Ventilation Safety Group will consider air flow strategies which achieve the most effective ventilation of occupied spaces. This requires that all factors such as air flow rate, mixing and distribution, dilution, thermal buoyancy and the impact of occupant movements must be considered. Hence, airflow patterns and ventilation rates can be evaluated using measurements of air velocities, indoor air quality (IAQ) monitoring and visual methods such as smoke tracing. In addition, computational Fluid Dynamics (CFD) modelling can be a useful tool to assist the ventilation design engineer to assess airflow patterns in the rooms where HEPA filter devices are to be located. CFD, particle tracing and other forms of airflow assessment can be used to identify the optimal locations to place devices.
Maintenance
All devices should undergo annual checks to ensure their correct performance. Filter replacement times should be optimised to allow for a straight-forward replacement schedule. A pre filter typically of grade ISO ePM10>50% should be installed within the unit to maximise the life of the HEPA filter. In healthcare environments the rule is to install devices with a filter lifetime of around 12 months. Some may last even longer and some operating in more contaminated environments or at higher humidity levels may need more frequent replacement. Devices should incorporate a dirty filter warning indicator or alarm for both the pre filter and the HEPA filter, to provide an easy visual indication to healthcare staff when a filter requires changing.
A Standard Operating Procedure (SOP) for each model must be in place for both replacing and safe disposal of used filters. Filter changes should follow the manufacturer guidance regarding the process and internal cleaning of the device. Filters should not be changed in clinical areas due to the possible hazards of microorganism and dust dispersal during the procedure. Those carrying out filter changes should wear appropriate PPE as agreed with infection control teams. Disposal of used filters requires a suitable risk assessment for safe bagging, handling and appropriate waste disposal for the used filter as it is potentially contaminated with pathogenic microorganisms.
Noise level
Air cleaner devices operated in occupied areas should have a sound level of ≤50 dB measured at 3 m (dB3m). For operations at boost setting, that might be used to purge a room, higher sound levels may be acceptable, however, this should be assessed based on the use of the room. Noise is a particular consideration when devices are positioned in rooms where patients are sleeping and lower sound levels than stated above may be required depending on local environmental conditions.
Safety Compliance
HEPA air cleaner devices used in healthcare settings have to comply with certain standards in line with medical applications and as a minimum with the Low Voltage Designated Standards. Other standards that should be followed are IEC 60601, a standard which applies to medical electrical equipment and medical electrical systems that ensures that HEPA filter devices used, recognise and mitigate risks to patient and user safety within a medical environment. CE and UKCA marking confirms that the product has been assessed to meet high health, safety, and environmental requirements. Lastly, electrical safety should be as well in compliance with IEC 60601 standards following Class I regulations and electrical wiring should follow IET Regulations BS 7671:2018.
Conclusion
We welcome the new NHS guidelines and standards on HEPA filter devices which are in line with our technology and brand values. Recognising HEPA filter air cleaners as a regulated solution in the Healthcare industry will enable NHS trusts to immediately confront ventilation challenges without having to modify estates. The new guidelines and standards represent an improvement opportunity for the NHS to raise ventilation performance in older healthcare facilities or any other areas to comply with HTM-03-01 extending operations of the existing infrastructure, which may have been on the red list.
Finally, it is undoubtedly noticeable that stand alone portable or semi-mounted devices, which were too long seen as the last solution, are climbing up the ladder due to their undeniable outperforming benefits, which will soon convert them into the first choice of healthcare professionals.
